Introduction: Hemophilia is an X-linked bleeding disorder among whom the majority have chronic hepatitis C (HCV) from past factor infusion. With among the longest duration HCV infection, now 30+ years from their first factor infusion, better predictors of HCV outcomes are needed now that liver-based gene therapy is FDA-approved. While antiviral therapy clears HCV viral load and reduces end-stage liver disease (ESLD), it may not reverse fibrosis/ cirrhosis or prevent hepatocellular carcinoma (HCC). We, therefore, studied the natural history of HCV in a well-characterized cohort of men with hemophilia and HCV to determine HCV prevalence and cumulative incidence of ESLD, HCC, and mortality.
Methods: This was a retrospective cohort study of 121 men with HCV and hemophilia cared for at the Hemophilia Center of Western PA, whose medical outpatient charts were reviewed under University of Pittsburgh IRB exempt determination, #21100086. HCV outcomes, including ESLD, HCC, platelet count (PLT)<100,000 (100K) u/L, and mortality were analyzed by age, ethnicity, HIV status, hemophilia type, inhibitor status, and antiviral therapy. Liver biopsies available on 32 patients were assessed for steatosis, Knodell, Ishak and Metavir scores. Fisher's exact test was used to compare outcomes by discrete variables. Kaplan Meier time to event analyses log-rank test was used to determine time-to-event outcomes for HCC and mortality, and logistic regression was used to determine variables predictive of HCV outcomes.
Results: The mean duration of HCV infection in 121 subjects was 54 years (range: 36-80 yr). Of these, 48 (39.6%) had received antiviral therapy (IFN-based or DAA-based): of those untreated, most died prior to its availability. A total of 31(25.6%) were HIV+, 24 (19.8%) had ESLD, and 7 (5.8%) had HCC. Among the 34 (25.9%) who died, ESLD was the cause in 11 (32.3%), HCC in 6 (20.6%), bleeding in 9 (26.5%), sepsis in 3 (8.8%), and AIDS, Parkinson disease, intravenous drug use, and suicide in 1(2.9%) each. The overall prevalence of ESLD was 0.365 per 100 person-years (py); PLT<100K, 0.173 per 100py; HCC, 0.106 per 100 py; and HCV-associated mortality, 0.335 per 100py.
Significant risk factors for ESLD included PLT<100K/uL, OR=6.159, p=0.014; HIV infection, OR=3.883, p=0.001; and age>50, OR=2.460, p=0.023. No antiviral-treated subject developed ESLD, p=0.001. The presence of ESLD was the most significant predictor of HCC, OR=11.476, p=0.003. An elevated Knodell score was a significant predictor of HCC, OR =2.450, p=0.044, while an elevated Ishak score was a significant predictor of ESLD, OR 1.930, p=0.030. Neither Metavir nor steatosis scores were predictive of ESLD or HCC, and no score was predictive of HCV mortality.
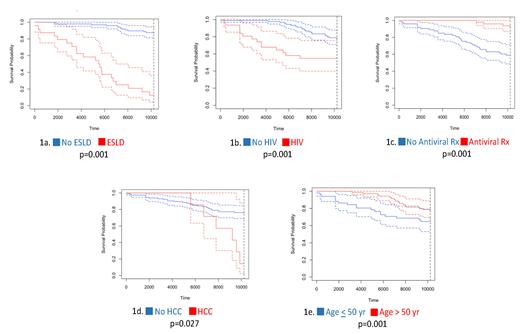
Kaplan Meier time-to-event survival analysis for all-cause mortality, 95% confidence interval (dotted lines) based on ESLD, HIV, treatment status, HCC, and age is shown in Figure 1a-1e. The overall mean ± SE (standard error) survival from initial HCV infection was 8890 ± 240 days. Comparing ESLD with non-ESLD, mean survival was 5321 ± 649 vs. 9773 ± 152 days, p=0.001 (Fig. 1a); for HIV+ vs. HIV-, 7032 ± 676 vs. 9530 ± 178 days, p=0.001 (Fig. 1b); for antiviral-treated vs. untreated, 10210 ± 19 vs. 8094 ± 365 days, p=0.001 (Fig. 1c); for HCC vs. non-HCC, 8433 ± 614 vs. 8918 ± 251 days, p=0.027 (Fig. 1d); and for age > 50 vs. ≤ 50 yr , 9588 ± 173 vs. 8052 ± 460 days, p=0.001 (Fig. 1e).
The cumulative incidence (CI) of ESLD was 16.86% overall. Comparing HIV+ vs. HIV-, ESLD-CI was 41.44% vs. 7.36%, p= 0.001; in antiviral-treated vs. untreated, 0% vs. 27.08%, p=0.001; in age > 50 vs. ≤ 50 yr, 13.10% vs. 14.03%, p<0.001; and in PLT<100K/uL vs. PLT≥100K/uL, 48.15% vs. 1.61%, p<0.001. The HCC-CI was 2.88% overall, including in HIV+ vs. HIV-, 0% vs. 3.71%, p= 0.27; in antiviral untreated vs. treated, 2.00% vs. 3.85%, p=0.760; in age > 50 vs. age ≤ 50, 5.63% vs. 0% , p=0.040; and in PLT<100K/uL vs. PLT ≥ 100K/uL, 33.3% vs.1.61%, p=0.001. HCC-CI was similar between those with vs. without ESLD, 6.67% vs 2.04%, p=0.27.
Conclusion: ESLD in people with hemophilia and HCV is associated with increased risk of mortality, HCC, and PLT<100K. The risk for ESLD is increased in those with HIV and antiviral untreated. HCV remains an important cause of major morbidity and mortality in this cohort of people with hemophilia and HCV, despite antiviral therapy. This suggests ESLD, HCC, HIV, PLT<50K/uL, and antiviral Rx assessment before hemophilia liver-based gene therapy.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal